Claiming for community nursing services
Overview
Only DVA contracted Community Nursing providers can claim for the delivery of community nursing services to DVA clients.
DVA contracted Community Nursing providers can claim for services retrospectively at the end of each 28-day claim period, using the Community Nursing Schedule of Fees. These are the set fees that compensate DVA contracted Community Nursing providers for the costs associated with the provision of community nursing services in each 28-day claim period.
All claims for community nursing services are processed and paid through Medicare (Services Australia) on behalf of DVA.
As a contracted provider, it is your responsibility to ensure that your Community Nursing provider number is current and to check the eligibility of each DVA client before you provide services.
Back to topProvider numbers
Community Nursing providers are allocated a provider number by DVA that must be used when claiming for community nursing services. A new provider number may be allocated where there is a change in provider legal entity, ABN, address or other circumstances. It is a provider’s responsibility to notify DVA when any changes occur and for DVA to determine if a new provider number is required.
The current active provider number must be used when claiming for community nursing services. Claims for services may be rejected by Medicare when an inactive provider number is used.
Back to topHow to claim for services
Each claiming period is 28-days and starts from the date the client first receives face to face services.
Determining the core item
There are three categories of visit – clinical care, personal care and other care. Claiming for services is based on the majority of care provided to each client and this determines the core item (either clinical care or personal care). Where the same number of visits for clinical care and personal care occur in a single claim period, the core item is considered clinical.
Determining the visit length
The Schedule of Fees categorises visits by the length of time required for each visit and these are also separated into clinical care, personal care and other care.
Add up the total minutes for clinical care and personal care services delivered over the 28-day claim period and divide each by the number of visits. The average length of visit and number of visits then determines the item numbers you claim on the Schedule of Fees.
For example:
- 450 clinical care minutes divided by 10 visits = 45 minutes
- 240 personal care minutes divided by 8 visits = 30 minutes
- Most visits are clinical therefore the clinical care core table is referred to in the Schedule of Fees and item NL14 chosen. The personal care visits will be from the personal care add on table and item NT02 chosen.
Determining the item numbers
Once the visit length, core and add-on items are determined correctly, additional item numbers for other services that were required and have been delivered in the same 28-day claim period (e.g. palliative care add on or overnight care) can be identified in the Schedule of Fees and submitted to Medicare.
Quick Reference Guide
A Quick Reference Guide for claiming has been developed to provide key information, further definitions and contact numbers. You can use this guide to assist in determining the correct item number/s to claim.
You can download a copy of the Community Nursing Claiming - Quick Reference Guide.
Ready Reckoners
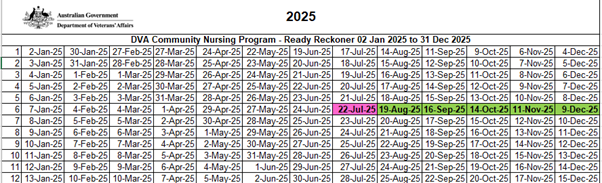
Ready Reckoners assist providers in determining the correct dates for each 28-day claim period and avoid rejected claims from Medicare. The Ready Reckoner shows day 1 of each 28-day claim period.
How to use the Ready Reckoner:
- select the date services commenced for the client (this is day 1 of the 28-day claim period)
- the dates in the columns to the right show the next date (day 1) of the subsequent claim periods
- The example in the table below highlights day 1 of the first 28-day claim period in pink and day 1 for the subsequent periods in green
The first visit to the client was on 22 July 2025 therefore the 28-day claim period is 22 July 2025 to 18 August 2025. The next claim period commences on 19 August 2025 and so on.
2025 Ready Reckoners:
2024 Ready Reckoners:
Back to topSubmitting a claim for payment
Claims for payment can only be submitted to Medicare at the end of the 28-day claim period.
There are currently two options available for claiming DVA Community Nursing services. Online claiming is the preferred option and enables the fastest method of payment.
Medicare Online claiming
Providers can submit online claims using Medicare compliant software only, with the list of compliant software and vendors available on the Services Australia website Software developers for Medicare Online. Not all software is compatible for use in claiming Community Nursing Services.
Medicare Online claiming provides a streamlines system for the lodgement of claims, including a digital record for lodgements. Online claiming can result in faster actioning of claims for payment of services.
In addition, Minimum Data Set (MDS) information is captured using the software and submitted automatically with online claiming.
Further information on Medicare online claiming can be found on the Services Australia website: DVA education for health professionals.
Manual claiming
Manual claiming requires Community Nursing providers to complete hard copy forms and vouchers (listed below) for each client and then submit these via post to Medicare for processing. The forms cannot be submitted via email.
In addition to completing the claim and voucher forms, Community Nursing providers who submit manual claims must also complete the Minimum Data Set (MDS) Collection Tool. Once completed, the tool must be submitted separately via email to DVA at mds@dva.gov.au.
Back to topTimeframes for claiming
As per the Notes for Community Nursing Providers, claims for payment of community nursing services, regardless of the claiming method used, must be lodged with Medicare for processing within six months of the first day of the 28-day claim period.
In addition, the Health Insurance Act 1973, section 20B(2)(b), states that a Medicare claim must be lodged with Medicare within two years of the date of service.
Late lodgements due to poor record keeping, inadequate staffing, resources or training, or any issues with record keeping software will not be accepted after the two-year timeframe.
Back to topLate claims
As advised on the provider claims page, DVA can accept claims up to two years from the date of service.
Claims greater than 2 years from the first day of the 28-day claim period will result in a rejection by Medicare.
Claims greater than two years from the date of service can only be considered if the provider can:
- show us that if we do not assess your claim, you may suffer financial hardship
- provide us with documents that prove you may suffer financial hardship.
If you are seeking to lodge a late claim with DVA, please call 1300 550 017.
Back to topMinimum Data Set
DVA requires all providers to submit data on all the community nursing services delivered to each client. This data is referred to as the Minimum Data Set (MDS).
For providers who use Medicare Online claiming, this information is uploaded automatically when providers submit their claims to Medicare.
For providers who claim manually, data must be entered into the Minimum Data Set (MDS) collection tool and once completed, submitted separately via email to mds@dva.gov.au.
Refer to the Notes for Community Nursing providers and the MDS Collection Tool – Quick Reference Guide for further information:
- MDS Collection Tool - Quick reference guide (PDF 1.3 MB)
- MDS Collection Tool - Quick reference guide (DOCX 820 KB)
Enquiries
For all general community nursing claiming enquiries (not including rejected claims), contact DVA Provider Enquiries on 1800 550 457.
For claims that have been rejected in Medicare, contact Medicare on 1300 550 017 (option 2).
For all other community nursing claiming enquiries (e.g. item codes, additional travel) contact the Community Nursing Program team at nursing@dva.gov.au.
Back to top